SPARC2 projects are developing next generation tools and technologies to inform future neuromodulation therapies
The vagus nerve is a bioelectronic highway that carries two-way electrical signals between the brain and many other organs of the body. The “lanes” of this highway are composed of over a hundred thousand nerve fibers. The use of a device to initiate or modify electrical signals in the vagus nerve, called vagus nerve stimulation (VNS), is under study as a therapeutic strategy for a wide range of conditions, including heart failure and inflammatory diseases. This type of therapeutic approach to modify electrical activity in nerves is broadly called neuromodulation. Current VNS technology stimulates the entire nerve, hitting all the fibers in the hope of activating the right ones. The therapy could be improved by selective stimulation of specific fibers to induce the desired therapeutic response, while avoiding or minimizing side effects. To do this, we need more information about how the vagus nerve fibers are organized. The NIH Common Fund’s Stimulating Peripheral Activity to Relieve Conditions (SPARC) program supports efforts to map these fibers so they can be targeted more specifically by neuromodulation therapies like VNS.
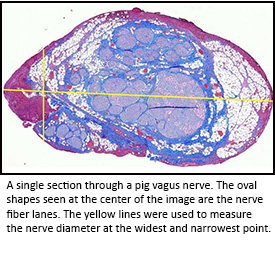 A SPARC-supported research team led by Dr. Warren Grill at Duke University is building simulations that predict which fiber lanes on the vagus nerve highway will be activated by different patterns of electrical pulses. To work well, these models need to be fed anatomical data such as size, number, and location of the fibers within the vagus nerves in humans and in appropriate animal models. In a newly published study, lead author Megan Settell and colleagues from Dr. Kip Ludwig’s group at the University of Wisconsin-Madison, along with Dr. Warren Grill’s group at Duke, used careful dissection, labeling, and analysis to chart the different lanes of fibers along the vagus nerve highway in pigs. They even identified areas along the vagus nerve highway that may contribute to unwanted side effects when electrodes are placed there. Their findings are helping improve predictive VNS simulations that may pave the way to new devices, placement strategies, or stimulation protocols, adding up to more effective VNS therapies in the future.
A SPARC-supported research team led by Dr. Warren Grill at Duke University is building simulations that predict which fiber lanes on the vagus nerve highway will be activated by different patterns of electrical pulses. To work well, these models need to be fed anatomical data such as size, number, and location of the fibers within the vagus nerves in humans and in appropriate animal models. In a newly published study, lead author Megan Settell and colleagues from Dr. Kip Ludwig’s group at the University of Wisconsin-Madison, along with Dr. Warren Grill’s group at Duke, used careful dissection, labeling, and analysis to chart the different lanes of fibers along the vagus nerve highway in pigs. They even identified areas along the vagus nerve highway that may contribute to unwanted side effects when electrodes are placed there. Their findings are helping improve predictive VNS simulations that may pave the way to new devices, placement strategies, or stimulation protocols, adding up to more effective VNS therapies in the future.
Read more about this work in a news article from the University of Wisconsin-Madison.
Reference
- Functional vagotopy in the cervical vagus nerve of the domestic pig: Implications for the study of vagus nerve stimulation. Settell M, Pelot NA, Knudsen BE, Dingle AM, McConico AL, Nicolai EN, Trevathan JK, Ezzell JA, Ross EK, Gustafson KJ, Shoffstall A, Williams JC, Zeng W, Poore SO, Populin LC, Suminski A, Grill WM, Ludwig K. J Neural Eng. 2020 Feb 27.


