With just a blood sample, a new tool can be used to accurately diagnose non-small cell lung cancer (NSCLC) and assess whether patients would respond well to a targeted immunotherapy treatment. NSCLC represents 80-85% of lung cancer, which is the third most common cancer type diagnosed in the U.S. and the leading cause of cancer‐related death.
The new prediction tool was developed as part of Common Fund’s Extracellular RNA Communication program.The program focuses on developing technologies to understand and harness the therapeutic potential of RNA circulating in the body outside of cells, known as extracellular RNA (exRNA), including how it may serve as a marker to better understand diseases like cancer.
The immune system responds to cancer by activating immune cells that work together to kill tumor cells. But many tumors have found a way to evade the immune system by producing a protein called programmed death-ligand 1 (PD-L1). When PD-L1 binds to a protein found on immune cells called PD-1, it keeps those cells from killing the PD-L1-containing cancer cells. Drugs that bind to PD-L1, stopping it from binding to PD-1 on immune cells, can restore the ability of the immune system to kill tumor cells. However, this form of cancer immunotherapy doesn’t work for everyone. Patients with higher levels of PD-L1 in their tumors generally have better response rates to immunotherapy, so the gold standard method for predicting whether an NSCLC patient is a candidate for immunotherapy measures PD-L1 levels from a tumor tissue biopsy sample. Because cancer cells within a tumor can be variable and sampling at a single site may not represent the entire tumor, tissue biopsies only predict 20%-40% of NSCLC patients who will respond well to immunotherapy.
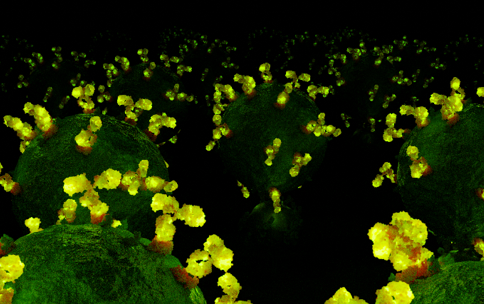
To improve these predictions, researchers led by Eduardo Reátegui, Ph.D., at The Ohio State University, engineered a gold‐based biochip to measure exRNA and proteins found within and on the surface of extracellular vesicles (EVs). EVs are tiny molecular containers that carry RNA and proteins throughout the body and are known to play a role in communication between cells. EVs can be shed from tumors and circulate in the bloodstream, so their characteristics and cargo, including exRNA, can provide insight into the features of a tumor. The new technology can sort and isolate individual EVs and measure both PD-1 and PD-L1 proteins, as well as PD-1/PD-L1 RNA, providing a more comprehensive picture of PD-L1 production within the tumor compared to a single tissue sample.
By sorting EVs from patients’ blood and measuring proteins and exRNA cargo from individual EVs, the researchers found that the tool predicted whether a patient had NSCLC 93.2% of the time. It also predicted immunotherapy response with an accuracy of 72.2%, exceeding the current gold standard method, suggesting that this tool may be a better and less invasive way than tissue biopsies for predicting response to immunotherapy.
Reference: Nguyen LTH, Zhang J, Rima XY, Wang X, Kwak KJ, Okimoto T, Amann J, Yoon MJ, Shukuya T, Chiang CL, Walters N, Ma Y, Belcher D, Li H, Palmer AF, Carbone DP, Lee LJ, Reátegui E. An immunogold single extracellular vesicular RNA and protein (AuSERP) biochip to predict responses to immunotherapy in non-small cell lung cancer patients. J Extracell Vesicles. 11(9):e12258. doi: 10.1002/jev2.12258.


